With over five billion medical claims processed annually, the healthcare industry faces immense pressure. As healthcare demand increases, the complexity of claims processing also increases, leading to significant challenges. Healthcare providers are overwhelmed by repetitive tasks, leaving little time for patient care, while insurers struggle with increasing claim denials and fraudulent activities.
Those inefficiencies delay reimbursements and put a lot of strain on providers and insurers, which leads to longer wait times and inaccurate billing.
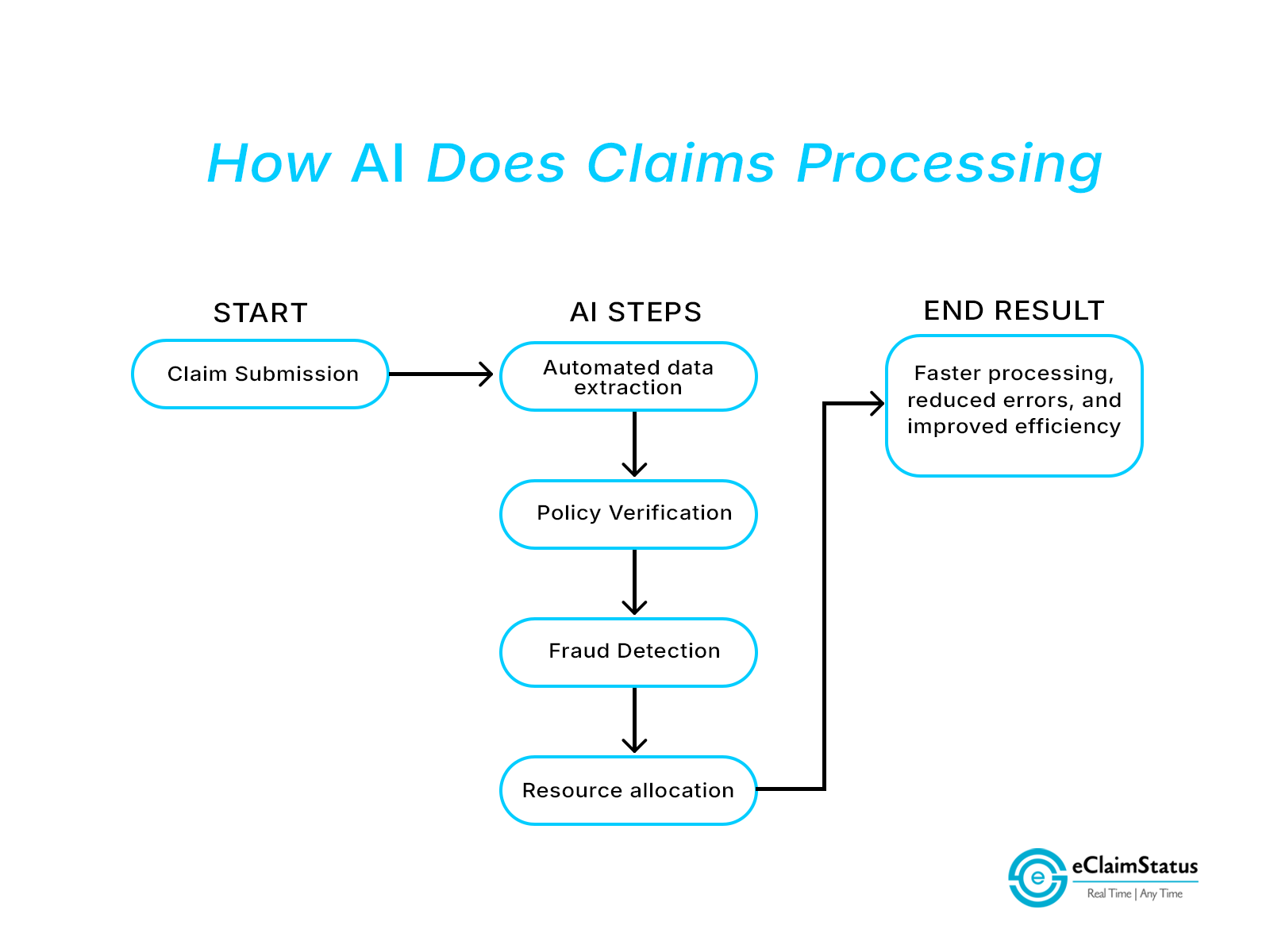
AI-driven automation presents a hopeful solution that is capable of accelerating the claims process and reducing stress for everyone involved. In this blog, we will look at how AI aids in claims processing, its effects, and the future of automated medical claims using AI.
The Current Challenges in Claims Processing
Managing medical claims is complicated, and old methods struggle to meet the needs of today’s healthcare. Here are the key challenges faced by patients, providers, and payers.
High Claim Volumes
As more people get healthcare and insurance, the daily number of claims increases. Traditional systems struggle to handle this volume, causing delays in approvals and creating backlogs.
Repetitive Manual Tasks
Administrative tasks like checking documents, confirming policies, and handling claims take much time and energy. Healthcare providers spend a large part of their time—sometimes as much as one-sixth of their working hours in such repetitive processes. It can cause mistakes, such as data errors and missing paperwork, resulting in claims denials and expensive corrections.
Increased Error Rates
Human mistakes like wrong data entries, missing details, or overlooked information during checks can result in claim denials. Each denied claim creates problems—time lost in fixing issues, delayed payments, and tension between providers and payers.
Why Is There A Need for AI in Claims Processing?
AI can process large amounts of data to spot patterns such as fraud and waste early, greatly boosting efficiency. A McKinsey report shows that improved data use could save up to $100 billion each year by making decisions better and simplifying clinical trials and research.
Automate Administrative Functions
The manual process of medical claims is time-consuming, leading to increased claim denials and financial strain on providers. AI directly tackles these issues by automating routine administrative tasks. For example, AI systems can extract data from electronic health records (EHRs) and verify insurance coverage instantly. This reduces administrative burdens, minimizes errors related to manual data handling, and accelerates claims processing.
Improve Fraud Detection and Resource Optimization
AI’s predictive capabilities are transforming fraud detection and resource optimization. AI-driven systems have achieved notable accuracy rates, with some models reporting up to 94.6% accuracy in detecting fraudulent claims. This significantly enhances the reliability of the claims process and helps prevent fraud before it occurs.
Improving Resource Allocation
AI not only handles routine tasks but also provides insights into claim trends and resource demands. By predicting claim volumes and identifying bottlenecks, insurers can allocate resources more effectively, avoiding backlogs and ensuring compliance with regulatory deadlines. This lowers operational expenses and enhances connections with providers and policyholders.
How AI-Powered Claims Automation Helps Patients, Providers, and Payers
AI is advancing quickly and bringing major benefits to everyone in the healthcare system. By automating everyday tasks and increasing efficiency, AI is changing how providers, payers, and patients navigate the claims process.
- For providers, AI lessens administrative work, giving them more time to focus on patient care. With quicker claims processing, providers receive payments faster, which helps improve revenue management.
- For payers, automation helps payers save money by cutting down on mistakes and lessening manual tasks. AI-driven fraud detection reduces fake claims, enhancing efficiency in operations.
- For patients, quicker claims processing means faster treatment approvals and fewer billing problems, which increases satisfaction and trust in healthcare services.
The Future of AI in Claims Automation
AI-driven claims automation is set to change the healthcare field by fixing inefficiencies, simplifying processes, and providing quicker, smarter solutions. Insights from HLTH 2024 highlight the progress and future possibilities of AI in this area.
Predictions for the Next 5–10 Years
At HLTH 2024, top innovators showcased how AI is transforming claims processing. A key tool is Natural Language Processing (NLP), which pulls important details from unstructured data such as medical records and patient notes. Additionally, Machine Learning (ML) enhances predictive analytics, allowing insurers to evaluate claim results and spot irregularities. This change has led to real-time processing, removing the delays seen with older methods.
The Role of AI in Creating End-to-End Solutions
AI will provide smooth, end-to-end claim automation, covering everything from the first submission to the final payment. Tools such as smart document scanning, automatic approvals, and fraud detection help maintain both precision and speed. At HLTH 2024, NVIDIA showcased how AI-driven virtual agents could further enhance this process by providing real-time support and guiding patients through claim preparation.
Smarter Healthcare Ecosystems
The future of AI-driven claims automation is about building a connected healthcare system. In this system, claims processes, Electronic Health Records (EHRs), and decision-support tools will work together smoothly. This connection will change the disjointed methods into a streamlined workflow that helps everyone involved. Claims approvals, policy changes, and payment processes can happen in a shared digital space, minimizing delays and conflicts.
The healthcare industry is moving from reacting to claims issues to managing them proactively. This change will create a new standard for efficiency, accuracy, and teamwork. The idea of a connected future is close at hand—AI technologies are leading the way, and new opportunities are growing quickly.
AI for Smarter and Faster Healthcare Claims
AI-driven claims automation is more than a fix for current problems; it is the base for a quicker, smarter, and more connected healthcare system. The future of AI-driven claims automation will build a system where claims processing integrates smoothly with other healthcare technologies. Tools like real-time data analysis and fraud detection are already paving the way for smarter decisions and better outcomes
Leave your insurance eligibility verification to eClaimStatus. Get started with your 15-day free trial, call us at 310-294-9242 or write to us sales@eclaimstatus.com
