In radiology, processes such as billing, insurance claims, submissions, follow-ups, denials, etc. are very time-consuming and labor-intensive along with the long line of patients and the tough treatment procedures. Prior Authorization is the icing on the cake, adding to your already full administrative burden. This process is intended to ensure appropriate care, but the challenges that come with managing prior authorizations have become endless for radiology services.
In recent data, 88% of physicians have reported that they must dedicate two full business days to doing 45 PAs per week and state that they face high or extremely high administrative work owing to prior authorization. In the same report, a concerning 46% of them said that PA led to delays, further escalating the patients’ healthcare needs and resulting in them getting urgent or emergency care.
As a care provider, this can affect your bottom line: delayed care, claim denials, and valuable time diverted to paperwork instead of focusing on the patients. It can also mean that your patients don’t get the care they deserve due to process delays/ denials.
What’s the way out?
Prior Authorization Automation can give your service a significant edge considering all the hurdles of doing PA paperwork. Several healthcare providers have stated that automating radiology PA and admission notices has reduced write-offs and resulted in higher success rates for getting approvals. How do automation tools help decrease PA denials? Let’s find out.
Benefits of Prior Auth Automation
For a simple comparison of how the prior authorization process is typically carried out vs how automation benefits the provider, check out the table below:
| Traditional Prior Authorization Process | Automation of Prior Auth Verification |
| Manual data entry and submission | Digital, real-time communications |
| Phone calls and fax communications | Integrated payer connectivity |
| Staff dedicating 2+ days a week to auth tasks | Significant reduction in staff time required |
| Time-consuming payer portal navigation | Improved accuracy and consistency |
| High risk of human error | Faster turnaround times (hours to days) |
| Lengthy turnaround times (days to weeks) | Lower denial rates (clinical, admin, timely filing) |
| Higher denial rates due to errors/missed deadlines | Automated status tracking and updates |
| Automated data extraction and submission | Streamlined patient care pathways |
| Frequent follow-ups and status checks | Reduced administrative burden on staff |
| Staff burnout from repetitive tasks | Enhanced patient satisfaction and experience |
| Delayed patient care and scheduling | Rich analytics for continuous improvement |
| Patient frustration with delays and uncertainties | Digital, real-time communications |
| Limited data insights for process improvement | Integrated payer connectivity |
Key Features of Prior Auth Automation Systems
PA automation works on different areas of patient data from registration to getting approval for their treatment procedures, making the process easy and more time-efficient. The following are the various features that come with this system:
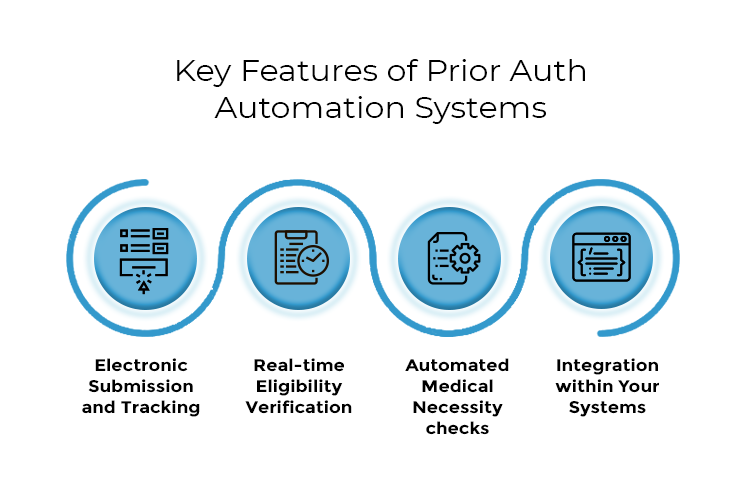
Electronic Submission and Tracking
At the core of Prior Auth automation is electronic submission and tracking of patient data. It digitizes the process, automatically compiling patient and procedure information into standardized forms for payer submission. This reduces manual data entry errors and substantially reduces the burden on your staff.
Real-time Eligibility Verification
Real-time eligibility verification acts as a proactive safeguard, automatically checking patient coverage and plan-specific benefits when appointments are scheduled. This helps prevent claim denials and ensures necessary authorizations are in place before imaging or treating the patient.
Automated Medical Necessity checks
By incorporating and staying up-to-date on the current clinical guidelines and payer criteria, automated medical necessity checks prompt for the relevant clinical information and cross-check it against the stored guidelines. This increases the likeliness of first-time submission approvals and reduces the delays in prior authorization.
Integration within Your Systems
For a seamless transition to automated processes, integration of the application with your existing systems is crucial. By directly connecting with your current EHR, PMS, and RIS, and pulling relevant data, the software feeds authorization status back into these systems and updates them regularly. You can eliminate the efforts on duplicate data entry with this integration and provide a unified and simple-to-use workflow.
Implementation Strategies for Automating Prior Auth Verification
While automating your Prior Auth Verification processes can save your staff’s time and efforts significantly, it is also important to train them for the automated workflow initially to avoid any issues in the future. We have outlined the implementation strategies:
- Map your current prior authorization process, identify bottlenecks, and gather staff input on challenges.
- Research and select a radiology-specific solution that’s compatible with your IT infrastructure and scalable for future needs.
- Develop a comprehensive training plan, providing hands-on practice and addressing concerns about the new system.
- Designate “super users” to support your colleagues during and after implementation.
- Establish baseline metrics before implementation to measure the impact of automation.
- Track key performance indicators like turnaround times and approval rates post-implementation.
- Regularly review system usage and staff adoption to ensure optimal utilization.
- Collect ongoing feedback for continuous improvement and optimization of the automated system.
Use Case Examples
Example 1: Large hospital system implementation
If you are a large hospital system with multiple locations, prior authorization automation streamlines the workflow across all facilities. The automated system can quickly determine which procedures require authorization, and automatically submit requests when needed.
This reduces manual work for staff and helps with scheduling patients more efficiently, reducing wait times. By reducing authorization-related delays and denials, the hospital system can also improve its revenue cycle and patient satisfaction.
Example 2: Outpatient imaging center
If you run a busy outpatient imaging center, prior authorization automation can help manage increasing patient volume. With the help of the automated system, you can handle routine authorizations quickly, and fasten the turnaround times for more efficient scheduling.
Automating Prior Auth Verification also helps reduce errors in the process, leading to fewer claim denials, and yet again results in improved cash flow and revenue collection for your center. On top of this, you can enhance the patient experience by reducing scheduling delays and administrative burdens.
Enhance Efficiency and Reduce Denials in Radiology with Prior Auth Automation
In conclusion, prior authorization automation offers significant benefits for radiology practices, including increased efficiency, reduced denials, and improved patient care.
eClaimStatus provides a comprehensive solution for automating your prior authorization processes. Leveraging advanced technology and a vast payer network, it simplifies your workflow. Our user-friendly platform offers real-time eligibility verification, automated submission, and status tracking, all while ensuring HIPAA compliance.
Take the next step in optimizing your radiology practice – explore eClaimStatus’ prior authorization automation solution today.
Leave your insurance eligibility verification to eClaimStatus. Get started with your 15-day free trial, call us at 310-294-9242 or write to us sales@eclaimstatus.com
