Prior Authorization Automation Services: Save Time and Reduce Errors
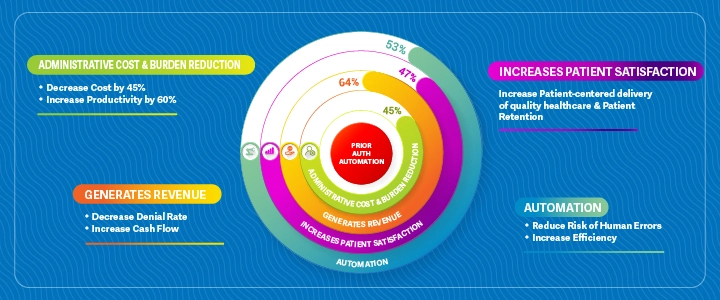
Prior authorization is a process that Healthcare Providers must follow to obtain approval from Health Insurance Companies before they can proceed with certain medical procedures, treatments, or medications. The process can be time-consuming and frustrating for both Patients and Providers. As healthcare costs continue to rise, Medical Providers are looking for ways to reduce the administrative burden of Prior Authorization (PA). Our Prior Authorization Automation Service aims to simplify this process by automating many of the steps involved.
Automated PA solutions streamline the entire process by providing end-to-end support from eligibility verification through follow up with payers on status updates.
Prior Authorization Process
Healthcare Environments
Manual insurance verification burdens front office staff and leads to costly errors, with 30% of denials linked to coverage issues. eClaimStatus Insurance Verification Software automates this process, reducing mistakes, improving cash flow, boosting point-of-service collections, and enhancing patient satisfaction—delivering measurable improvements within just 30 days of implementation.
Fetch patients’ eligibility & benefits information from over 900+ payers in seconds on one platform. Single or Multiple claims, get real time status in seconds. Optimize your revenue by routing each claim to the correct payer on timely basis.
Get instant, updated insurance claim status for single or multiple patients in seconds. Take timely action for effective claims denial management. Optimize your practice’s revenue by eliminating payment risks. Save time and money by getting rid of long hold over phone.
eClaimStatus Insurance Discovery Software combines 25+ years of revenue cycle expertise with advanced, technology-driven algorithms to uncover previously unknown, missed, or uncollected commercial and federal coverages. This powerful blend of human insight and automation ensures accurate coverage identification, optimizing reimbursements and improving overall revenue cycle performance.
eClaimStatus streamlines Mental Health Insurance Verification by providing real-time eligibility and benefits information across 800 payers. This reduces wait times and phone calls, improves administrative efficiency, ensures accurate patient responsibility collection, and allows front-office staff to focus more on patient care—enhancing both operational savings and patient satisfaction.
eClaimStatus simplifies Physical Therapy Insurance Verification with real-time access to eligibility and benefits from 900 payers. It reduces phone calls, eliminates wait times, and ensures accurate patient responsibility collection. This boosts administrative efficiency, allowing providers to spend more time delivering personalized patient care and enhancing overall clinic productivity.
eClaimStatus enhances Emergency Room Insurance Verifications by streamlining front-office workflows, reducing delays, and improving the patient experience. By addressing key challenges that impact satisfaction, it helps boost HCAHPS scores and strengthens your hospital’s reputation—ensuring better outcomes for both patients and your overall practice.
eClaimStatus streamlines insurance verification for Chiropractic care by offering real- time access to eligibility and benefits across 800 payers. It reduces wait times and phone calls, improves administrative efficiency, and ensures accurate patient responsibility collection—allowing providers to focus more on personalized chiropractic care and enhancing overall patient satisfaction.
eClaimStatus simplifies Insurance Discovery for Ambulance Billing by identifying active patient coverages and determining correct coverage hierarchy. This ensures accurate claim routing to the appropriate payer, helping EMS providers reduce denials, improve billing performance, and increase revenue—while continuing to deliver critical emergency medical services efficiently.
Insurance verification is essential for successful healthcare reimbursement. Verifying coverage at the time of scheduling ensures patients have active insurance, helping prevent claim denials or rejections. Skipping this step can lead to revenue loss, making timely insurance verification crucial for maintaining your practice’s financial health and operational efficiency.
eClaimStatus © All Rights Reserved | Privacy Policy | Terms of Use | Security Notice
 sales@eclaimstatus.com
sales@eclaimstatus.com 310-294-9242
310-294-9242